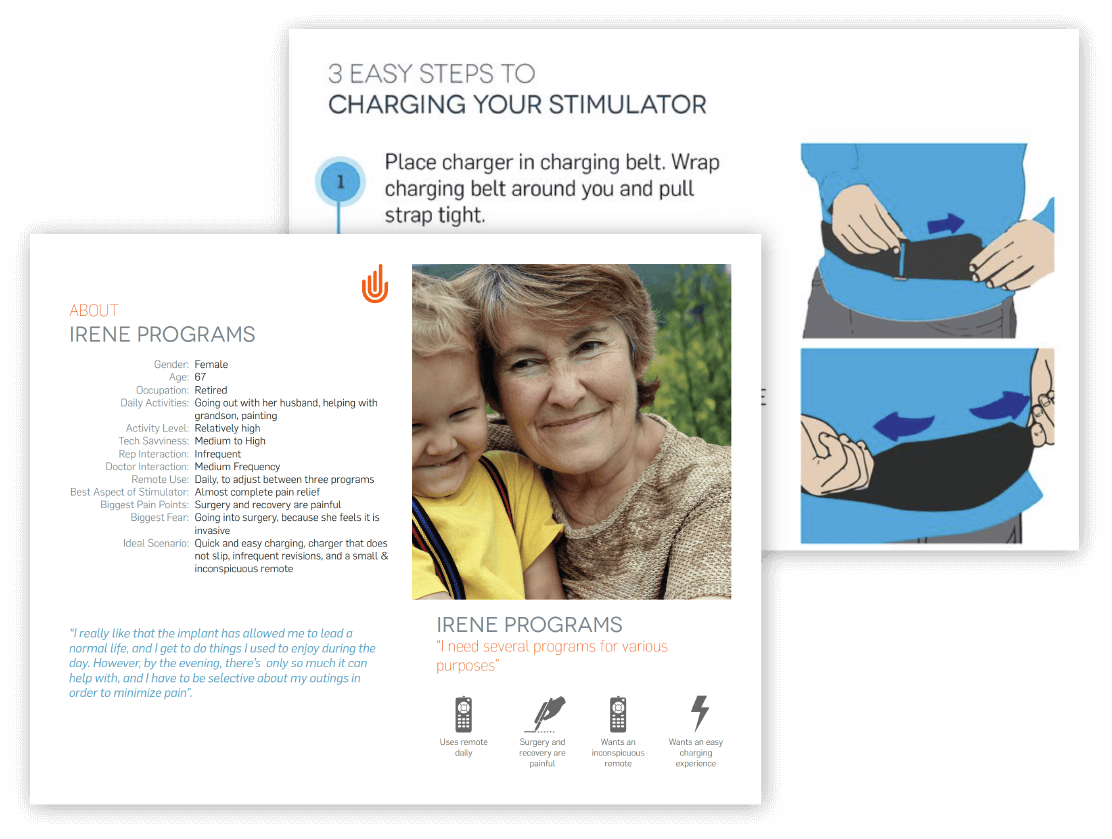
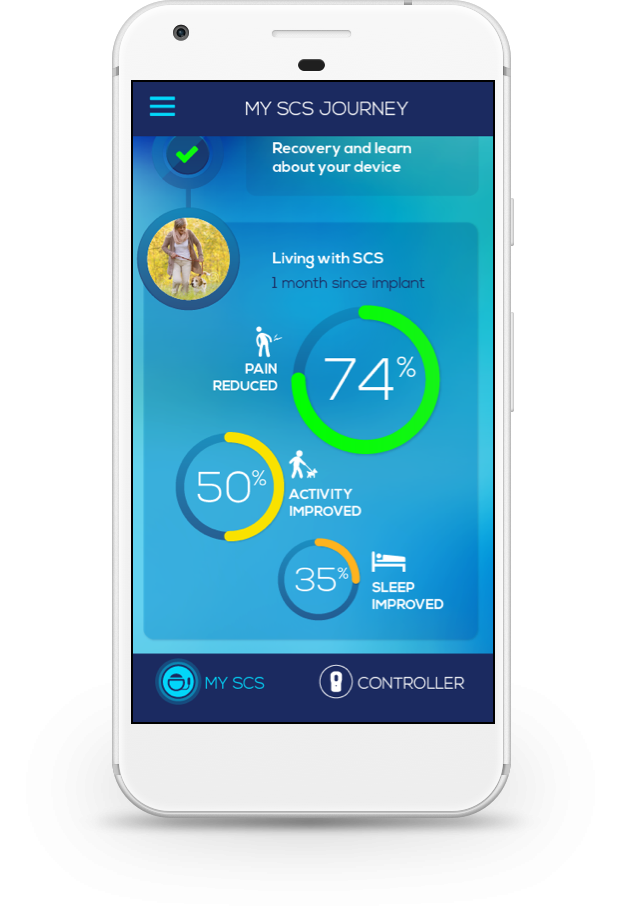
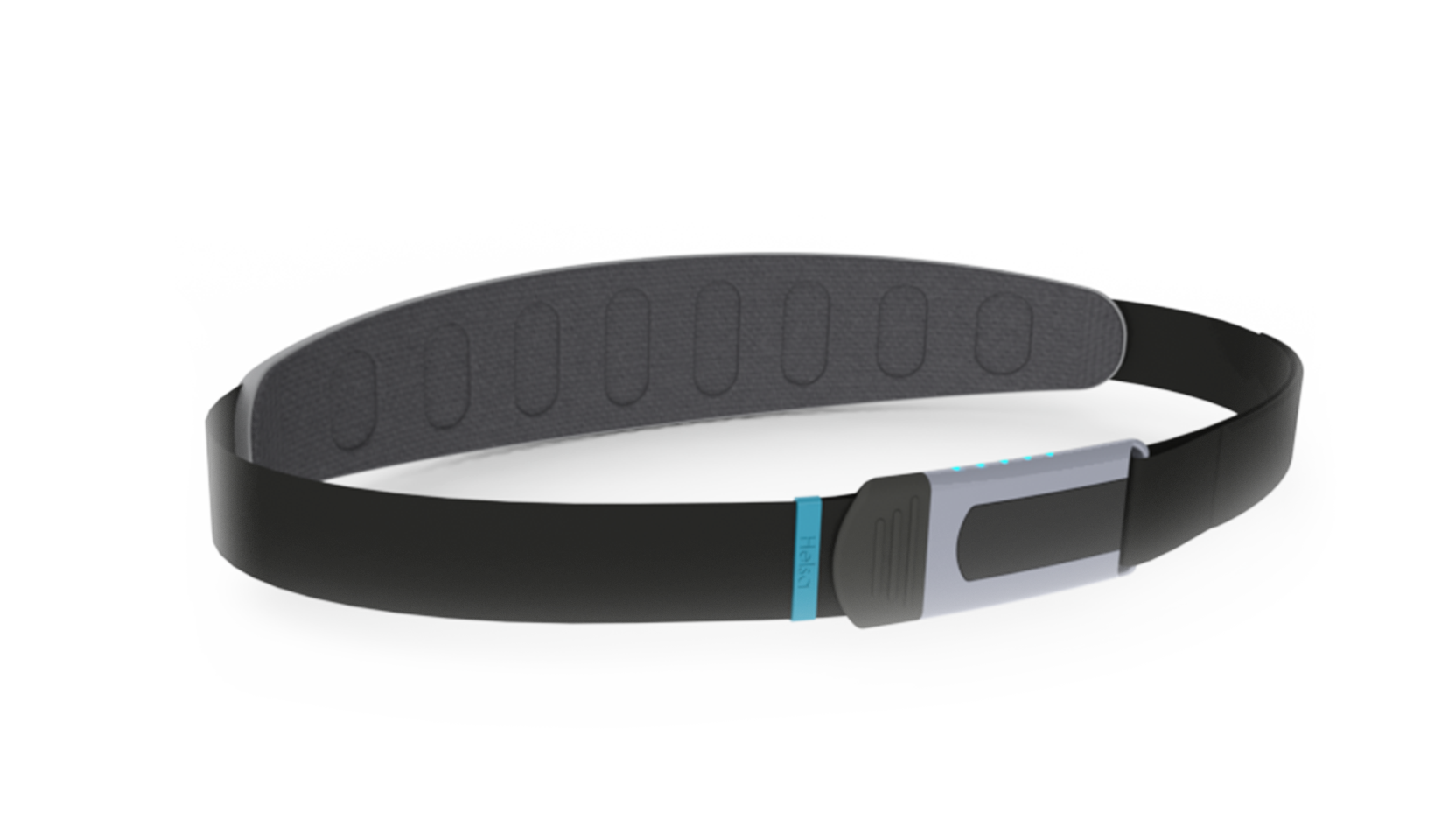
Boston Scientific Neuromodulation (BSN) was looking to start early development of a next-generation medical implant to provide effective therapy for Chronic Pain and Parkinson’s Patients.
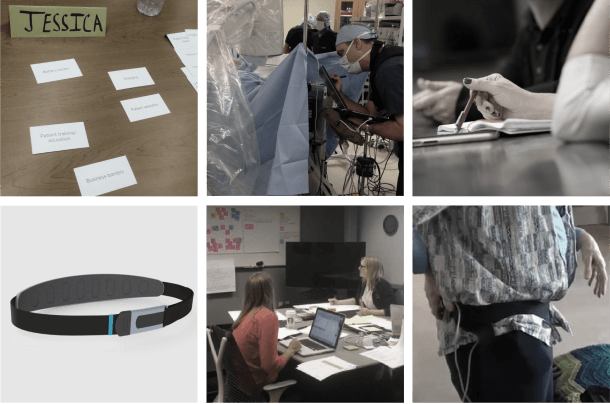
In order to best understand the existing unmet needs and size preferences, we attended surgeries and programming sessions, as well as conducted Focus Groups and Interviews with Surgeons, Chronic Pain and Parkinson’s Patients, Caregivers and Sales Reps. Following the rounds of research, designs for the remote, implant and software surrounding the experience were explored and refined.